ABOUT PMI SCIENCE
PMI Science: Transparency and Scientific Rigor Behind PMI's Smoke-Free Products
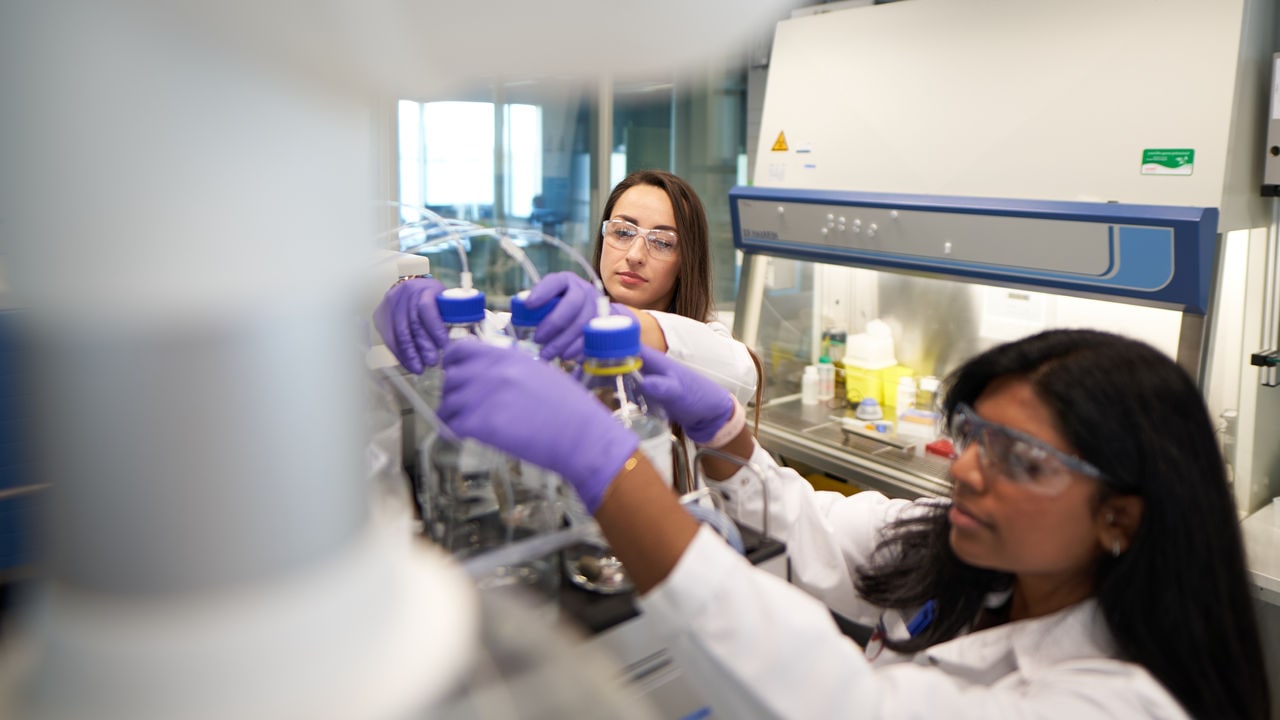
At PMI Science, our aim is to decrease the impact smoking has on public health, which is the essence of tobacco harm reduction. We do this by developing and assessing better alternatives to cigarette smoking–alternatives that don't burn tobacco–following rigorous scientific methods.

Get in touch
We would be happy to hear from you
Whether you have a question, a comment, or an idea, send us a message. Open dialogue is something we are passionate about, and we would like to know your views.